Role of ZFP57 in regulating Imprinted Genre Expression in Human Rhabdomyosarcoma.
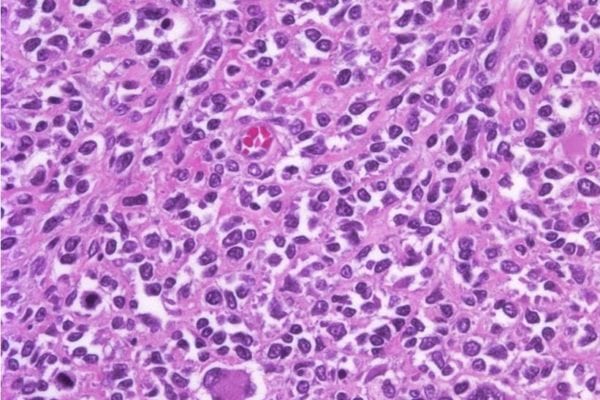
Rhabdomyosarcoma (RMS) is the most common soft tissue sarcoma in children and young adults. Current therapy has long-term side effects and achieves cure in less than 40% of metastatic patients, a feature that has not changed over the past 40 years. The two main subtypes of RMS, Embryonal (ERMS: 70% of cases and more prevalent in <10 yo), and Alveolar (ARMS: less prevalent and with poorer prognosis), have abnormally increased expression of a subset of paternally imprinted genes. Amongst those, IGF2 (Insulin-like Growth Factor-2, that promotes IGF pathway), DLK1 (Delta-Like 1 homolog, that promotes NOTCH pathway) and RasGRF1 (Ras Protein-Specific Guanine Nucleotide-Releasing Factor 1, that promotes RAS pathway) have proven to participate in development, growth and metastasis of RMS.
Imprinting is a mechanism of gene regulation in which a selected group of genes are exclusively expressed from either copy inherited from the mother or from the father, and is crucial for normal embryonic growth and development. Imprinted genes are usually organized in clusters. An Imprinting Control Region (ICR) located within the cluster controls the expression or silencing of these genes. ZFP57 (Zinc Finger Protein-57) specifically binds ICRs in embryonic cells maintaining imprinted gene expression during embryonic development. ZFP57 expression decreases as cells differentiate and is normally absent in tissues after birth.
In our lab, we developed a mouse model of rhabdomyosarcoma and imprinted gene expression is increased, as it is in human ERMS. More over, we detected, for the first time, expression of ZFP57 not only in murine ERMS, but also most importantly in human cell lines (4) and primary tumors (20) of from both types of rhabdomyosarcoma. We will test in our proposal that expression of imprinted genes in RMS relies on ZFP57. We are currently using genomic editing tools and gainof-function approaches to increase or decrease ZFP57 in RMS cells. If we prove ZFP57 is responsible for imprinted gene expression, blocking its function would tackle simultaneously multiple relevant pathways in RMS. Since ZFP57 expression is normally limited to embryonic stages and it specifically regulates imprinted gene expression, blocking this mechanism should not harm normal mature cells, leading to improved outcome with less toxicity.
Principal Investigator:
Estibaliz Lopez Rodrigo MD
Clinical Fellow
Joyner Lab – Department of Developmental Biology
Sloan Kettering Institute
Rm. 721, Rockefeller Research Labs
430 E. 67th St, NYC NY 10065
212-639-3980
Slotkin Study

Emily Slotkin, MD Over the past forty years, intensive combinations of chemotherapy, surgery, and radiation have helped to improve outcomes for those afflicted with rhabdomyosarcoma, but for patients with disease that has spread or does not respond well to these therapies, this aggressive cancer remains very difficult to treat. New methods to attack rhabdomyosarcoma are urgently needed. In our laboratory we are working to change this with the following projects:
1. Rhabdomyosarcoma is sometimes caused by an abnormal genetic event where portions of two chromosomes inappropriately fuse together only in tumor cells. This abnormal event causes changes in cells that result in their rapid and uncontrolled division, making them cancerous. Ideally, medications would kill cells only having these genetic changes, while leaving other healthy cells unharmed. Such specificity is not achievable with standard chemotherapies, and thus far there have been no new medications able to target the genetic changes in rhabdomyosarcoma cancer cells only. In our laboratory, we are working to change this by pioneering several innovative methods to directly target the inappropriately fused chromosomes and thereby kill rhabdomyosarcoma cancer cells. We have developed drugs which identify the malignant cells with extreme precision and impair their function at a basic level. Using compounds which alter RNA, one of the basic building blocks of cells, we are developing new drugs called antisense oligonucleotides. This extremely powerful but exact approach has enormous potential to affect the fundamental biology which we know drives some types of rhabdomyosarcoma cells to grow out of control. Rigorous testing of these drugs is ongoing, and it is the goal of all of us working daily on these novel technologies that they will soon provide more effective and less toxic treatment options for everyone suffering from rhabdomyosarcoma or similar cancers.
2. Research at Memorial Sloan Kettering Cancer Center has shown that treatment with a group of drugs called mTOR inhibitors are very effective for certain adult patients with cancer. The promise of these drugs has yet to be realized for children. Recent work from our laboratory shows that mTOR inhibitors may be particularly effective for children with rhabdomyosarcoma. Currently, we are working with several pharmaceutical companies that manufacture these agents to open a clinical trial that will test these drugs in children.
3. Despite intensive laboratory work, there have few new treatments for rhabdomyosarcoma over the past 20 years. Many people suspect that this may be because our methods of studying pediatric cancers are inefficient and imprecise. To combat this problem, we are using a new method to edit the genetic codes of the cells that we use in our laboratory experiments. This incredibly powerful and innovative tool allows us to precisely change the genome of cells we are testing to better match those of the patients we treat. We hope that these techniques will make our experiments more accurate and therefore more quickly lead to the discovery of effective treatments.
Dela Cruz Study

The PaulieStrong Foundation Research Summary – Filemon Dela Cruz MD.
My experiences in the laboratory and the clinic, caring for children with cancer, have served as the foundation for my goal to identify and develop effective therapies for pediatric sarcomas. We have entered a new era of medicine where we can utilize new techniques and technologies, that barely existed a decade ago, to identify the biological “weak spots” of various sarcomas and other cancers. By identifying the specific vulnerabilities for any given sarcoma, we can employ the existing clinical armamentarium of drugs to target, treat, and cure children of their cancer.
To accomplish this goal, our laboratory has been at the forefront of developing and testing unique experimental models of childhood sarcomas including the “avatar” mouse model where we “grow” a biologic replicate of each patient’s tumor. By using these avatar models, we can not only test a large number of potentially effective drugs and identify the most effective agents for use to the patient, but we would also be helping to create invaluable models of rhabdomyosarcoma and other childhood sarcomas and solid tumors for future research efforts. Support from The PaulieStrong Foundation will enable our goal of bringing these innovative tools and approaches to finding cures for all children living with cancer.
2800000 3000000 94
